- Home
- Mind & body
- Women may experience different heart attack symptoms from men
At CBHS we help you manage your health challenges. We believe in offering you the services, support and tools you need to live your best life.
Health and Wellness Programs are available to support eligible members towards a healthier lifestyle. Each Health and Wellness Program is subject to its own eligibility criteria.
Contact us for more information and to confirm your eligibility for a program.
Women may experience different heart attack symptoms from men

Women have poorer outcomes than men after a heart attack
Heart disease is the leading underlying cause of death for Australian men, and the second most common cause of death for women. But the potential difference in heart attack symptoms can have deadly consequences for women.
‘Women have poorer outcomes than men following a heart attack,’ says Natalie Raffoul, who is the risk reduction manager at Australia's Heart Foudndation.
Men are twice as likely to have heart attacks compared with women, but women are three times more likely to have a fatal heart attack. In 2019 almost half (45%) of all heart attack deaths were in women.
There’s a mistaken belief that women don’t have heart attacks
‘Many people mistakenly believe only men have heart attacks, not women,’ says Natalie.
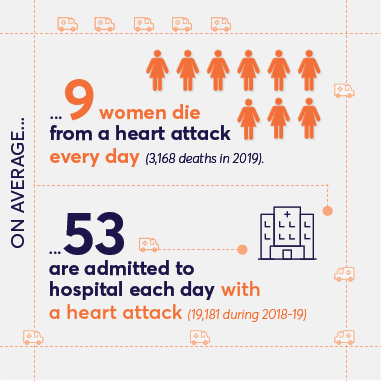
- On average, 9 women die from a heart attack every day (3,168 deaths in 2019).
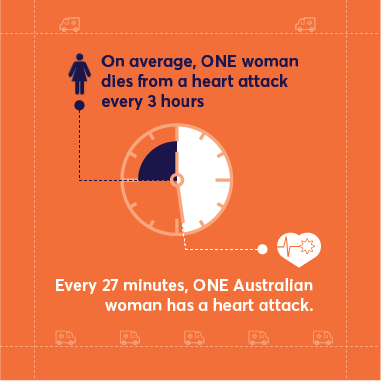
- On average, 1 woman dies from a heart attack every 3 hours.
- In 2019, almost half (45%) of all deaths from heart attack were women.
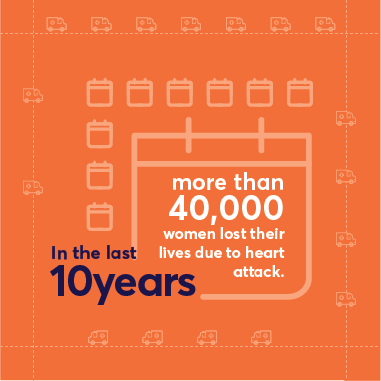
- In the last 10 years, more than 40,000 women lost their lives due to heart attack.
- On average, 53 are admitted to hospital each day with a heart attack (19,181 during 2018-19).
- Every 27 minutes, one Australian woman has a heart attack.
‘Women are regularly confronted by stereotypes including that heart disease only affects older men or that chest pain is the only warning sign of a heart attack,’ Natalie adds.
Sixty-five-year old Alice was one of the lucky ones.
For several months the Sydney theatre professional battled unexplained fatigue. ‘I just felt so tired all the time. I put it down to a general lack of fitness.’

She was walking to rehearsals in Sydney one day when her symptoms worsened. ‘I felt odd pain in my jaw. I also felt a bit breathless.’
Alice explained how she felt on arrival, the director suggested they cancel, and Alice called an Uber to go home to rest.
‘I had something to eat then I lay down for a while.’
‘Even when they present to hospital, women are less likely to receive the same life-saving treatments as men.’
That evening Alice felt waves of pain coming and going in her neck and jaw.
‘Around two o’clock in the morning I began to feel real discomfort in my chest and armpits. It was nothing like the stabbing pain I assumed was associated with heart attacks.’
Thankfully, Alice was concerned enough to call an ambulance. Paramedics confirmed she was having a heart attack and, by four-fifteen that morning, she was being operated on at RPA, where surgeons inserted the first of three stents to unblock her arteries.
Again, Alice was one of the lucky ones.
‘Even when they present to hospital, women are less likely to receive the same life-saving treatments as men,’ says Natalie.
‘We associate heart attacks with crushing pain in the chest, but that’s not always the case for women.’
An estimated 510,000 Australian women live with heart, stroke or blood vessel disease (also known as cardiovascular disease), and heart disease kills more than twice as many women as breast cancer.
So, what are some of the warning signs of a heart attack that women might experience?
These are some common signs of heart attack in women
The fatigue and pain in her jaw that Alice experienced are not uncommon heart attack symptoms for women.
‘We associate heart attacks with crushing pain in the chest, but that’s not always the case for women,’ says Natalie.
The most common heart attack symptom for men and women is chest pain, but women are more likely than men to experience other symptoms, such as pain in the neck, back or jaw, shortness of breath, nausea or vomiting.
These heart attack symptoms can be more common in women:
- pressure or pain in the lower chest or upper abdomen
- extreme or unexplained fatigue
- pain or discomfort in the back, neck, stomach, or jaw
- feeling light-headed or dizzy
- pain or discomfort in one or both arms
- cold sweats, nausea, or vomiting
- shortness of breath.
According to the Heart Foundation, women are slower than men to respond to the warning signs of a heart attack, possibly because they’re less likely to experience the ‘classic’ symptoms of a heart attack.
If you or someone you are with experience the warning signs of a heart attack, call triple zero (000) immediately and ask for an ambulance.
Alice was a prime candidate for a heart attack
Women are thought to be better at looking after their health than men, but that isn’t the case when it comes to heart health
‘I hadn’t realised that I was a prime candidate for a heart attack,’ says Alice.
Alice wasn’t overweight and didn’t have diabetes, but she was an occasional smoker. She also took little exercise outside of rehearsals, and she had high blood pressure. Her own father had died of a heart attack at the age of 54.
‘I now realise that all those factors put me in a high-risk category.’
‘High blood pressure is one of the most important risk factors for both stroke and heart failure.’
Women are less likely to discuss heart health
Heart Foundation research suggests that women are less likely than men to have discussed heart health with their doctor in the past two years (33% versus 43%).
‘It just never occurred to me that my symptoms could be signs of heart disease,’ says Alice.
Women tend to develop symptoms of heart disease at a later stage than men. On average, they are diagnosed seven to ten years later than men. That’s because a woman’s risk of heart disease rises significantly after menopause.
Women are also less likely to receive advice on how to control or reduce the risk factors for heart disease (76% versus 85%).
More worrying still, women are also less likely to receive the same level of care in hospital if they do have a heart attack.
According to the Heart Foundation, the reasons for this are complex but lack of awareness, physical and hormonal differences in women, and unconscious bias in clinical decision-making are all part of the picture.
What can increase your risk of heart disease?
There is no single cause of heart disease, but several factors can increase your chance of developing it.
The risk factors you can’t control include age (your risk of developing heart disease increases with age) family history of heart disease, and complications during pregnancy (preeclampsia or gestational diabetes, for example, may increase your risk of heart disease later in life.)
Read more about heart health: Enjoy a healthy heart and healthy life (cbhs.com.au)
Other factors that can also increase your risk include:
- high blood pressure
- poor diet
- high cholesterol
- smoking
- lack of physical activity
- diabetes
- obesity.
How to reduce your risk of heart disease
Although Alice was a healthy weight, she admits she didn’t exercise much, and her diet wasn’t as good as it could have been. She was also a smoker, had high blood pressure and a family history of heart disease.
‘Now that I know the risk factors, I’ve given up smoking and I’m increasing my exercise. I’m also improving my diet.’You can reduce your risk of heart disease in a number of ways:
- Improve your diet
- Achieve and maintain a healthy weight
- Increase exercise levels
- Quit smoking.
These lifestyle changes can also benefit your overall health and may reduce your risk of diabetes and hypertension (high blood pressure).
Do you have hypertension?
High blood pressure is one of the most important risk factors for both stroke and heart failure. It’s sometimes referred to as ‘the silent killer’ because most people with high blood pressure have no symptoms.
Hypertension is two to three times more common in women than in men. Reducing hypertension can greatly reduce your risk of developing heart failure or stroke.
Lifestyle changes such as increased exercise, dietary improvements, limiting alcohol consumption and achieving a healthy weight can help treat mild hypertension.
Your GP can check for signs of hypertension. Medication may be required to treat more serious cases.
How can you look after your heart health?
The first step is to see your GP for a Heart Health Check.
If you’re a man or woman aged 45 and over, or an Indigenous Australian aged 30 or over, your Heart Health Check is subsidised by Medicare.
Heart Health Checks target people who haven’t yet had a heart event but who may be at risk of one. You can repeat the check every 12 months to monitor any changes in risk.
How old is your heart?
Did you know that your heart can age faster than you do?
Health professionals talk in terms of your ‘heart age’, and if that’s greater than your actual age, you may be at greater risk of a heart attack.
This simple quiz can calculate your heart age. The calculator is designed to be used by people between the ages of 35 and 75. It will help improve the accuracy of the results if you know your blood pressure and cholesterol levels.
Alice is one of the lucky ones
Alice has run through a gamut of emotions since her heart attack, from guilt and fear to depression and a sense of hopelessness. Ultimately, she’s relieved to have survived.
‘I know I’m one of the lucky ones,’ says Alice. ‘I have a friend whose mother felt exhausted one day, went for a lie down and never got up.’
If you experience any symptoms of a heart attack, call the emergency services on triple zero (000)
Find out more
You can find out more about cardiovascular disease in the Heart health section of our website.
All information contained in this article is intended for general information purposes only. The information provided should not be relied upon as medical advice and does not supersede or replace a consultation with a suitably qualified healthcare professional.
Sources:
Women and Heart Disease - Heart Research Australia
Australia's health snapshots 2020 (aihw.gov.au)
Cardiovascular disease in women, Summary - Australian Institute of Health and Welfare (aihw.gov.au)
Health and wellbeing
programs & support
You Belong to More with CBHS Hospital cover:
- Greater choice over your health options including who treats you
- Get care at home with Hospital Substitute Treatment program
- Free health and wellbeing programs to support your health challenges
Live your healthiest, happiest life with CBHS Extras cover:
- Benefits for proactive health checks e.g. bone density tests, eye screenings
- Keep up your care with telehealth and digital options
- Save on dental and optical with CBHS Choice Network providers