- Home
- Mind & body
- Intro to irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD)
At CBHS we help you manage your health challenges. We believe in offering you the services, support and tools you need to live your best life.
Health and Wellness Programs are available to support eligible members towards a healthier lifestyle. Each Health and Wellness Program is subject to its own eligibility criteria.
Contact us for more information and to confirm your eligibility for a program.
Intro to irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD)

Up to 30% of Aussies live with irritable bowel syndrome (IBS) right now, while Australia also has one of the highest rates of inflammatory bowel disease (IBD) in the world. With rates like these, it makes sense that as a nation we should be talking about gut issues a lot more – so let’s get right to the bottom (!) of it.
It’s easy to get confused between IBS and IBD, since both have very similar acronyms, symptoms, and affect our digestive system. But you’ll be surprised to know the two of them are actually quite different.
Let’s understand the underlying causes of these conditions, what makes them different from each other, and how we can live with them in a healthy way - with methods backed by science.
IBS and IBD – what’s the difference?
IBS is a disorder in our gastrointestinal (GI) tract that affects more women than men, usually before the age of 40 – studies say that one in five Australians will develop IBS in their lifetime.
IBS is considered a ‘functional disease’, which means, it’s trickier to identify as it has no visual signs. The typical investigation tools like blood tests, imaging, and endoscopy won’t show any abnormalities. IBS is diagnosed by exclusion – which means your doctor will have to rule out other possible diseases and conditions before diagnosing you with IBS. However, some exciting developments out of renowned Cedars-Sinai in the US mean that a blood test to provide a definitive diagnosis for IBS could soon be possible.
Meanwhile, IBD refers to inflammation, commonly of the large bowel ̶ but it can affect any part of your digestive tract (from mouth to anus) and will most often appear for the first time in people aged 15 to 30 years old.
IBD is what doctors call a ‘structural disease’ which means you can physically see the damage in your gut when looking at a scan, biopsy, colonoscopy, or endoscopy. IBD describes two main conditions ̶ Crohn's disease and ulcerative colitis, which are both autoimmune diseases. Ulcerative colitis, commonly referred to ‘colitis’, causes surface-level inflammation in your large bowel and rectum, while Crohn’s disease can cause inflammation anywhere in your digestive tract, and this can affect the entire thickness of the bowel wall.

What causes IBS and IBD?
When it comes to their causes, there is one main difference between them. IBS is triggered by environmental factors, while IBD is an autoimmune disease. The exact reason these autoimmune diseases develop is not known, but some important factors like genetics, infections, eating a ‘Western diet’ (a diet that is high in fat, sugar and processed foods), and smoking can play a role. It’s important to note that while stress and some foods can trigger symptoms, Crohn’s and colitis are not caused by diet or stress alone.
The direct cause of IBS is less clear, as it can vary from person to person. Food can play an important role and people may have different food triggers that can make their symptoms worse. But stress and lifestyle can affect you just as much. And that’s why usually your symptoms’ severity may change over time depending on which life stage you are in – periods of high stress will most likely worsen your IBS.
It’s also common to develop IBS after an episode of gastroenteritis, food poisoning, infections, illness, hormonal changes, or new medicines. It may also be due to a ‘miscommunication between your brain and your gut’.
The symptoms: IBD vs IBS
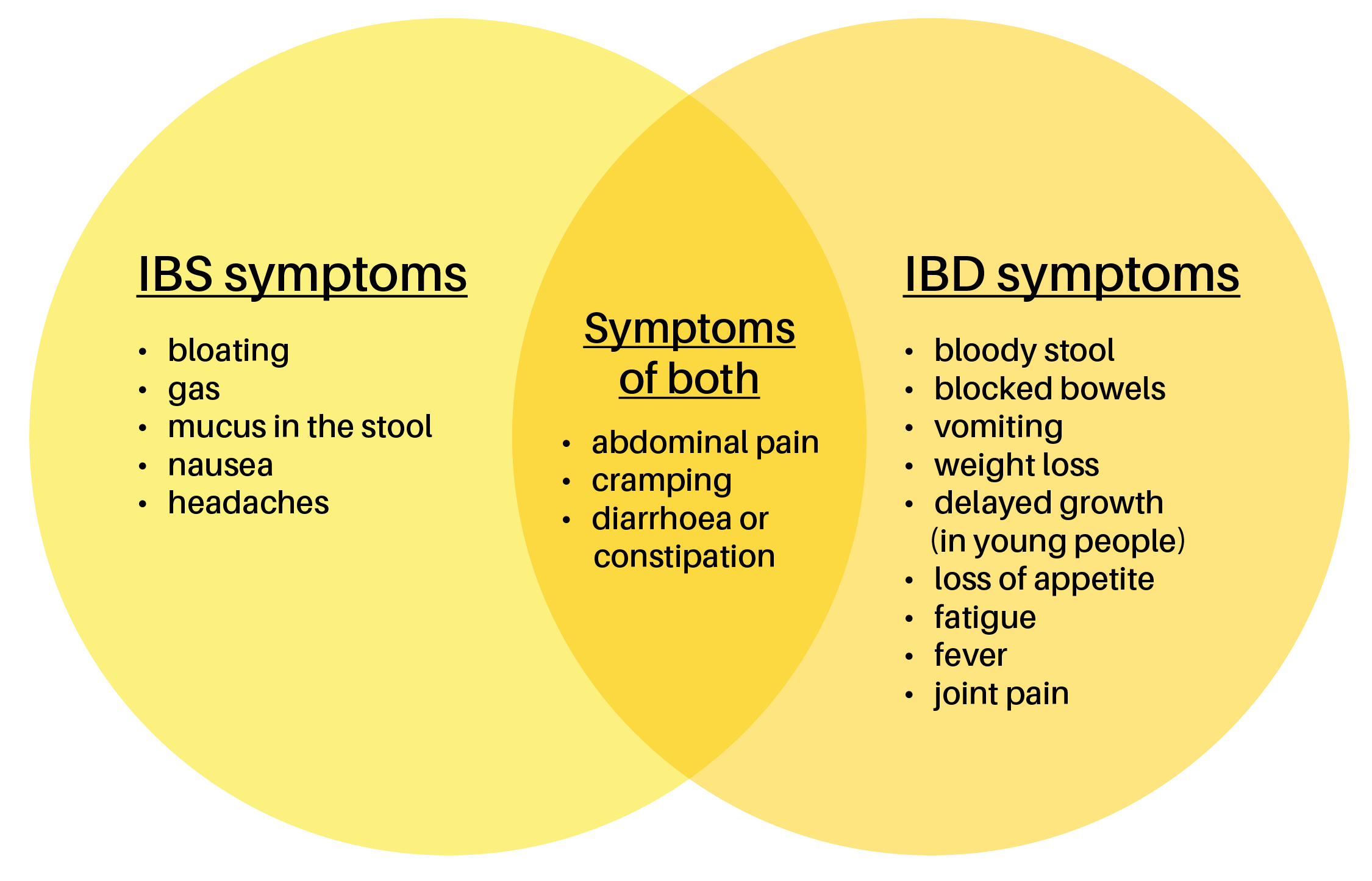
Because both are chronic conditions that affect the digestive system, IBS and IBD share some similar symptoms:
IBS is usually characterised by:
- abdominal pain
- cramping
- bloating
- wind
- diarrhoea or constipation (sometimes alternating between both)
- having to go to the bathroom more often or ‘right away’
With IBD, symptoms tend to get worse over time and may include any of the above as well as:
- bloody, mucousy or black stool
- unintentional weight loss
- mouth ulcers
- loss of appetite
- fever
- vomiting
- fatigue
- inflammation of your anus, skin, joints, or eyes
It’s particularly important to see your GP if you’re experiencing any of the symptoms of IBD.

Treatments and diets
Both IBS and IBD don’t have a permanent ‘cure’, instead they require a condition management plan, and IBS treatments usually are only needed from time to time – when you’re most triggered.
People with IBS often try changing their diet and lifestyle to manage their symptoms. There's no one-size-fits-all solution, so it’s best to ask your doctor and it may take a series of trial-and-error tests. Here is some general advice:
- add more fibre to your diet (sourced from food is always preferred but consult your doctor to see if supplements are a good idea)
- avoid lactose (found in dairy products) if it is a trigger for you
- cut down on foods that cause gas or bloating (usually beans and other legumes)
- drink more water or eat water-rich foods
- avoid caffeine (especially on empty stomach)
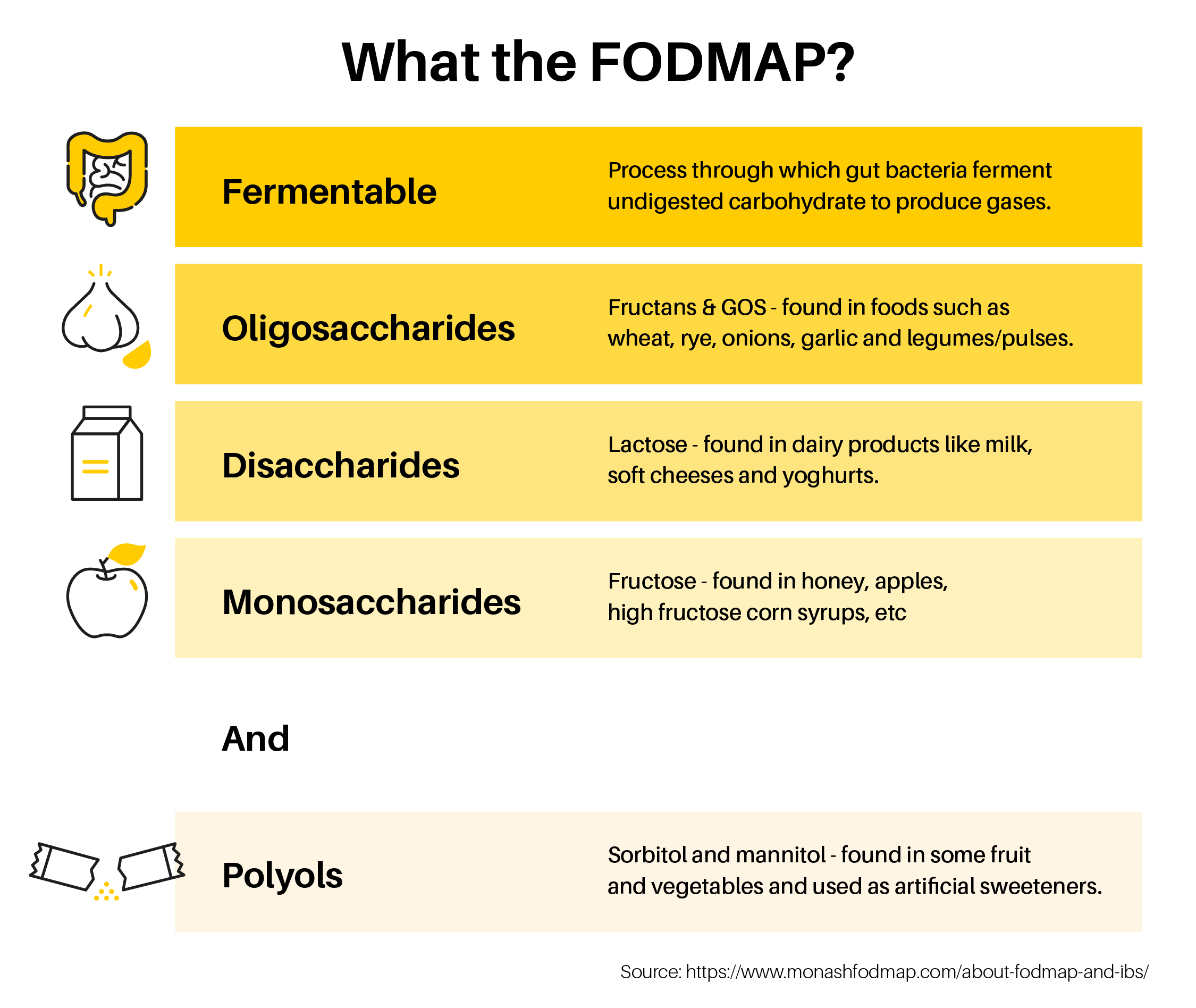
- limit or avoid FODMAPs (sugars found in some fruits, vegetables, breads, and dairy products).
- exercise regularly
- learn relaxation techniques to help reduce stress
- practise mindful eating
When it comes to IBD, you may need to both treat the symptoms and repair the damage on your digestive system. There are medications that can help target inflammation:
- aminosalicylates: help in mild or moderate cases by working on your intestine lining
- corticosteroids: suppress your immune system and are used for short-term flare-ups
- immunomodulators: affect your immune system and are used for long-term treatment
- biologic therapies: prevent proteins in your body from causing inflammation
- antibiotics: fight infections caused by the disease or surgery.
These medications generally don't work for IBS, that’s why it's so important to know which condition you have. Some people with IBD may need surgery to repair their digestive tract, but this isn't the case for IBS.
Also, for IBS, your doctor might suggest over-the-counter or prescription drugs to help with diarrhoea or constipation. These can include laxatives, anti-diarrhoeal, antispasmodics, and/or medications to manage other symptoms.
What is a low-FODMAP diet, how does it work, and is it for you?
The low FODMAP diet, developed by Monash University as a diagnostic tool, can reduce or help you manage some of the symptoms caused by your IBS or IBD.
A word of caution though. The diet isn’t recommended for long-term use, so consult your doctor or a dietitian if you’re considering FODMAP. Studies have shown that following a low FODMAP diet long-term can impact the composition of your gut microbiome because of the restricted intake of prebiotics.
Three in four people see improvements in IBS symptoms within weeks of adopting a low-FODMAP diet.
says Monash University.
But let’s go back to the beginning ̶ what is FODMAP? These are short-chain carbohydrates, found in some food, including wheat and beans, which are poorly digested in the colon. A low-FODMAP diet aims to identify your triggers, before reintroducing non-problematic foods into your diet.
A low FODMAP diet usually follows these three steps:
1- Swap high-FODMAP for low-FODMAP foods.
This stage will usually last around two to six weeks. It’s the most restrictive part of the diet, and usually the most challenging. But you should feel the results quite quickly.
2- FODMAP reintroduction
After your symptoms improve, it’s time to reintroduce FODMAPs into your diet. One at a time, over three days. An Accredited Practising Dietitian (APD) can guide you through a series of food reintroductions. These reintroductions can help work out which FODMAPs are triggering your symptoms and which ones are not.
3- FODMAP personalisation
After phase two, you’ll know which your body can tolerate and what foods are triggering your symptoms. That’s when your dietitian can build a personalised management plan. In the long-term this will be a balance between some FODMAP-rich foods that you can tolerate and some that you will avoid.
Here is a FODMAP diet guide to help you understand what foods are high and low FODMAP.
Top tip: you can also download the Monash University FODMAP app for some extra resources and support.
So, what else can you do to support your gut health?
Gut health is such a broad term nowadays, it’s important to use caution when it comes to the information available. It can be confusing and contradictory to say the least. It’s always worth checking whether claims are backed by science.
There is a rising movement for, and consumer interest in, probiotics and prebiotics to boost gut health. Monash University says that although we know that prebiotics and probiotics can alter a person’s gut microbiota, we still don’t know exactly how they affect our long-term health. It’s an area of research which is still emerging, and we look forward to following the developments in this space.
In the meantime, you can certainly try boosting your prebiotic and probiotic intake for yourself. For probiotics, there are a number of low-FODMAP, fermented foods to choose from, but here are a few examples:
- goat’s yoghurt
- tempeh
- sourdough spelt bread
- pickled gherkins.
You could also try small servings of sauerkraut, fermented red cabbage and pickled vegetables. Although they’re considered high in FODMAP, Monash University suggests that at smaller serving sizes these foods are low in FODMAPs.
Prebiotics are non-digestible fibres that promote the growth of good bacteria in the gut. For prebiotics you can try a firm unripe banana, small portion of canned lentils, ½ an eggplant, or a small tomato. They can be found in foods such as garlic, onions, leeks, asparagus, bananas, and oats. While prebiotics are great for promoting gut health, they can also cause digestive discomfort in people with IBS. Some people try adding supplements like Kfibre to their diet as a way to support gut bacteria without upsetting your stomach. We recommend checking with your doctor on whether a supplement could be right for you.
Other ways to support your gut:
- Eat more home-cooked meals for more control over the ingredients you’re putting in your body
- Reserve proper time to enjoy your meals. Eat slowly, chew well, and practise mindful eating
- Try building a stress management routine with techniques to help you, like nose breathing, relaxation techniques, and other small changes you can adopt to your day-to-day lifestyle
- Try the CBHS immunity-boosting routine.
Top take-aways tips
IBS and IBD symptoms can not only be painful but can really affect your quality of life. Health professionals are there so you don’t have to go it alone.
- See your doctor so they can rule out other bowel conditions and provide a professional diagnosis
- See a dietitian for personalised advice on managing IBS and IBD symptoms using dietary strategies
- Consult a dietitian before adopting a low-FODMAP diet. They can help to identify what might be triggering your symptoms. They can also help to make sure you are still getting enough fibre and all the nutrients you need.
Can we help you improve your gut health?
Dietitian support
If you hold any level of CBHS Extras cover, you can claim a benefit towards the cost of a dietitian. You can also claim a benefit on most levels of packaged cover.
Recipe ideas
You can find lots of healthy recipes on our website. They’ve all been tried and tested by CBHS nutritionists and dietitians, so they’ll taste as good as they look.
Feed your gut the food it loves to eat, and you’re likely to help your mind and your body feel better.
Get support for stress
The Stress section of our website has ideas and advice on practical ways to manage your stress at home. Try our blogs on 10 ways to reduce stress, how to beat stress with meditation, best healthy stress foods, and much more.
You can claim for recognised stress management programs under the Wellbeing benefits of your Extras cover. You can also claim benefits towards the cost of seeing a psychologist. Check your policy for more details or call us on 1300 654 123.
If you need help right now
If you or someone close to you needs help now, contact these services.
For crisis support:
- Lifeline on 13 11 14
- Suicide Call Back Service on 1300 659 467
For general mental health support:
- Beyond Blue on 1300 22 46 36
- MensLine Australia on 1300 789 978
- SANE Australia on 1800 18 7263
For medical support:
- Contact your GP or family doctor
- If it’s an emergency, contact 000
All information contained in this article is intended for general information purposes only. The information provided should not be relied upon as medical advice and does not supersede or replace a consultation with a suitably qualified healthcare professional.
Sources:
https://dietitiansaustralia.org.au/health-advice/irritable-bowel-syndrome-ibs
https://www.healthdirect.gov.au/crohns-disease
https://www.healthdirect.gov.au/irritable-bowel-syndrome-ibs
https://www.cedars-sinai.edu/research-education/research/departments-institutes/ibd-institute.html
https://www.healthdirect.gov.au/ulcerative-colitis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10302286/
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/irritable-bowel-syndrome-ibs
https://www.cbhs.com.au/mind-and-body/blog/what-s-your-poo-trying-to-tell-you
https://www.healthdirect.gov.au/low-fodmap-diets
https://www.cbhs.com.au/mind-and-body/blog/5-simple-ways-to-build-a-mindful-eating-habit
https://www.monashfodmap.com/about-fodmap-and-ibs/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6202292/
https://pubmed.ncbi.nlm.nih.gov/25016597/
https://www.monashfodmap.com/blog/fermented-foods-and-fodmaps/
https://www.cbhs.com.au/mind-and-body/blog/mindfulness-and-mindful-eating-an-activity-to-get-started
https://www.cbhs.com.au/mind-and-body/blog/stress
https://www.cbhs.com.au/mind-and-body/blog/top-ten-easy-ways-to-reduce-stress-and-improve-health
https://www.cbhs.com.au/member-health
https://www.cbhs.com.au/mind-and-body/healthy-recipes
https://www.cbhs.com.au/mind-and-body
https://www.cbhs.com.au/health-insurance/extras-cover
https://www.youtube.com/watch?v=2xc67pzHA1Q
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6175559/
https://www.cbhs.com.au/mind-and-body/stress
https://www.crohnscolitisfoundation.org/patientsandcaregivers/what-is-crohns-disease/treatment/medicationHealth and wellbeing
programs & support
You Belong to More with CBHS Hospital cover:
- Greater choice over your health options including who treats you
- Get care at home with Hospital Substitute Treatment program
- Free health and wellbeing programs to support your health challenges
Live your healthiest, happiest life with CBHS Extras cover:
- Benefits for proactive health checks e.g. bone density tests, eye screenings
- Keep up your care with telehealth and digital options
- Save on dental and optical with CBHS Choice Network providers
